Book Appointment
Find your preferred office location to set up an appointment with one of our specialists.
Our Doctors
FASMA is one of the largest groups of podiatrists in the United States.
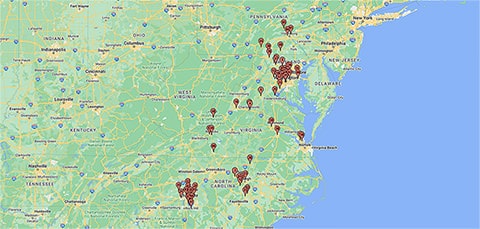
Locations
Enter your address to find a location near you.
Patient Portal
- Pay your bill online
- Request test results
- Manage appointments
- Send secure messages to your provider and the billing office
- Update your demographics
Commonly Treated Foot and Ankle Conditions
FASMA doctors provide a full scope of surgical and non-surgical treatment options, emphasizing open communication and education. It is FASMA’s aim to relieve every one of our patients of pain, and allow a return to a high level of function as quickly as possible.
Achilles Tendinitis
Achilles tendinitis is an inflammation of the tendon from acute overuse. The Achilles tendon is the largest tendon in the human body. It can withstand forces of 1,000 pounds…
Ankle Sprains
An ankle sprain occurs when the ankle twists, while walking or during physical activity, causing damage to the ligaments on the outside of the ankle. An audible “pop” may sometimes…
Arthritis of the Foot and Ankle
Osteochondritis dissecans (stiff ankle), presents as lesions that usually cause pain and stiffness of the ankle joint. Osteochondritis affects all age groups.
Bunion Deformities
A bunion is a bony prominence on the side of the foot at the base of the big toe joint. There is progressive movement of the big toe outward toward…
Corns & Calluses
The skin on your feet responds to friction and pressure by thickening. In some cases, the skin can become so thick that it begins to hurt. Skin that thickens without a core is called…
Custom Foot Orthotics
The normal arch functions as a shock absorber for our entire body. Each time we step down, we place up to five times our body weight onto the foot, depending…
Fractures
During the past 30 years, doctors have noted an increase in the number and severity of broken ankles, due, in part, to an active older population of “baby boomers,” according…
Fungal Toenails
Toenails that are discolored, thickened, brittle, and (sometimes) malodorous may have fungus.
Hammertoe Deformities
Hammertoes, mallet toes, and claw toes are all deformities describing bending or clawing of the toes. The toe ligaments and tendons tighten, causing a buckling of the toe joints.
Ingrown Toenails
Edges of toenails that press into the flesh can cause pain, swelling, redness, and even infection. Ingrown toenails start out hard, swollen and tender, and later, may become sore, red and…
Neuromas
A neuroma, sometimes referred to as a pinched nerve, is thickened nerve tissue that is benign in nature. This most often occurs between the third and fourth toes, which is…
Plantar Fasciitis (Heel Pain)
If you have pain under your heel, after sitting or sleeping and starting to walk, but it gets better as you walk around, you probably have plantar fasciitis. This is…
Warts
A wart is a callus-like growth on the skin caused by a virus. They can appear anywhere on the foot, but those to the sole of the foot are called…